Disabled Village Children
A guide for community health workers,
rehabilitation workers, and families
PART 1
WORKING WITH THE CHILD AND FAMILY:
Information on different Disabilities
B. Recognizing, Helping with, and Preventing Common Disabilities
CHAPTER 26
Leprosy
Hansen's Disease
What is leprosy? It is an infectious disease that develops very slowly. It is caused by germs (bacilli) that affect mostly the skin and nerves. It can cause a variety of skin problems, loss of feeling, and paralysis of the hands and feet:
|
|

|
painless ulcers of the feet |
How do people get leprosy? It can spread only from some persons who have untreated leprosy, and only to other persons who have 'low resistance' to the disease. It is probably spread either through sneezing or coughing, or through skin contact. Most persons who come into contact with leprosy have a natural ability to resist it. Either they do not get it at all, or they get a small unnoticeable infection that soon goes away completely.
From the time a person is first infected with leprosy germs, it often takes 3 or 4 years for the first signs of the disease to appear.
Leprosy is not caused by evil spirits, by doing something bad, by eating certain foods, or by bathing in river water, as some people believe. It is not hereditary and children of mothers with leprosy are not born with it. However, children who live in close contact with someone who has untreated leprosy are more likely to get it.
How common is leprosy? Leprosy is much more common in some parts of the world than others. It is more common where there are crowded living conditions and poor hygiene. But rich people can also get it.
Even with improved methods for treatment, today there may be more persons with leprosy than ever before. More than 12 million people have leprosy. In some villages in Asia, Africa, and Central America, 1 person in 20 has leprosy.
Can leprosy be cured? Yes. There are medicines that kill leprosy germs. Usually within a few days of beginning treatment, a person can no longer spread the disease to others. (in fact, most persons, when their leprosy is first diagnosed, can no longer spread it.) However, treatment in some persons must be continued for years to prevent the disease from coming back.
Is early treatment important? Yes. Early treatment stops the spread of leprosy to others. Also, if treatment starts before loss of feeling, paralysis, and deformities have appeared, recovery is usually complete and the person is not physically or socially disabled.
| Persons receiving regular, effective treatment do not spread leprosy. |
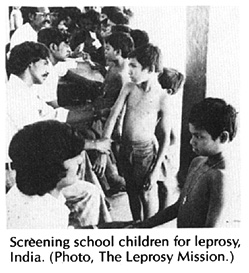
Checking children for signs of leprosy
In areas where leprosy is common, health and rehabilitation workers should work together with parents and schoolteachers to check all children regularly for early signs of leprosy. Most important are regular checkups of children in homes where persons are known to have leprosy. Checkups should be done every 6 to 12 months and should be continued for at least 3 years.
|
EARLY SIGNS A slowly growing patch on the skin that does not itch or hurt. The patch may be somewhat different in color from the surrounding skin. (Patches of leprosy are never completely white, and are not scaly, except during a reaction - see Page 219.) Note: In early skin patches, feeling is often normal, or nearly so. If feeling is clearly reduced inside a patch, leprosy is almost certain. |
|
WHAT TO LOOK FOR Examine the whole body for skin patches, especially the face, arms, back, butt, and legs.
If you find a slightly pale patch without a clear edge, keep watching the spot. Unless feeling is reduced inside the patch, look for other signs before deciding it is leprosy. (Many children have similar pale spots on cheeks and arms that are not leprosy.)
|
|
LATER SIGNS 1. Tingling, numbness, or some loss of feeling in the hands and feet. Or definite loss of feeling in skin patches. |
|
2. Slight weakness or deformity in the hands and feet.
|
|
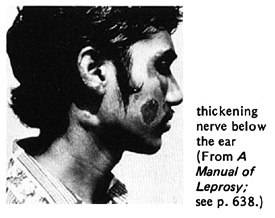
3. Enlargement of certain nerves, with or without pain or tenderness. The affected nerve feels like a thick cord under the skin. When they are quite thick, they may be easily seen. |
TEST INSIDE THE SKIN PATCHES FOR REDUCED FEELING. With the tip of a feather or stiff thread, lightly touch the skin inside and outside the patch and have the child tell you (without looking) where he feels the touch.
WARNING: Sterilize the needle in a flame before testing another child.
In a similar way, test for a numbness or reduced feeling in the hands and feet. |
|
Have the child straighten her fingers. If she cannot do this, it may be a sign of paralysis from leprosy.
Also have the child try to touch the base of her little finger with her thumb.
(CAUTION: These weaknesses may also be caused by polio, muscular dystrophy, or other problems.) |
|
Check for large nerves in these places. |
Diagnosing leprosy
Although skin patches are often the first sign of leprosy, many other diseases can cause similar patches. Only when there is a loss of feeling inside the skin patch, as compared with the skin outside the patch, can we be almost sure the person has leprosy. However, in some forms of leprosy, loss of feeling in skin patches may develop only years later, or not at all. Therefore, other evidence of leprosy must be looked for.
Another sign of leprosy - tingling, numbness, or loss of feeling in hands and feet- may also have other causes.
To make a fairly certain diagnosis of leprosy, the person should have at least 1 of these 3 major signs:
-
definite loss or change of feeling in skin patches
Note: Leprosy patches on face often do not lose feeling as much as on other parts of the body.
-
2. definite enlargement of nerves

(For nerves to check, see Page 216.)
-
3. presence of leprosy bacilli in a 'skin smear'
A 'split skin smear' is prepared by cutting a thin layer of skin from a skin patch. Less commonly it is taken from the moist skin deep inside the nose-an area that is often heavily infected. The skin sample is placed on a glass slide, colored with special stains, and examined with a microscope.

The bacteria (bacilli) of leprosy, if present, can be seen under the microscope.
Whenever you suspect leprosy but the diagnosis is uncertain, a 'skin smear' should be taken (by a trained worker).
Note: Not many persons with leprosy show all 3 of these signs. Persons with loss of feeling in skin patches usually have no bacilli in their skin smears.
Types of leprosy
Depending on how much natural resistance a person has, leprosy appears in different types. Here are the characteristics of the main types.
|
TUBERCULOID LEPROSY (TT)
|
|
'BORDERLINE' LEPROSY combines features of both tuberculoid and lepromatous leprosy.
Depending on where it falls along the line between the two extremes, borderline leprosy is divided into: borderline tuberculoid (BT), borderline (BB), and borderline lepromatous (BL). |
|
LEPROMATOUS LEPROSY (LL)
|
Leprosy reactions
Sometimes persons with leprosy have sudden periods of increased problems. These may be something like an allergic reaction to the leprosy bacilli. Leprosy reactions can happen in untreated persons, during treatment, or after treatment has stopped. Reactions can occur when there are changes in the body, such as puberty in boys, in late pregnancy or following childbirth, during illness from other causes, after vaccination, or at times of emotional stress.
There are 2 types of leprosy reactions:
Type 1 reactions happen in persons with borderline leprosy when the body increases its fight against the leprosy germs. There is danger of new weakness and loss of feeling.
Signs to watch for are:

- skin patches may become swollen and red
- swollen hands and feet
- new tingling or weakness of hands and feet
- pain or discomfort along nerves (Rarely, lumps along the nerves form sores and drain pus.)
|
IMPORTANT: Reactions sometimes cause new weakness and loss of feeling without nerve pain. |
Type 2 reactions happen with lepromatous leprosy. The body is reacting against too many bacilli.
Signs may include:
- swollen, reddish, or dark lumps under the skin, especially on the face, arms, and legs
- fever
- pain in testicles, breasts, or fingers
- stuffiness or bleeding of the nose
- red eye, with or without pain. Danger: This may lead to iritis or loss of vision unless treated early.
Rarely, this reaction causes death due to swelling of the mouth, throat or lungs, or to kidney problems.
|
IRITIS (INFLAMMATION OF THE IRIS)
Pain may begin suddenly or gradually. The eye waters a lot. It hurts more in bright light. There is no pus as with conjunctivitis. Vision is usually blurred. This is a medical emergency. Antibiotic ointments do not help. Get medical help. |
If untreated, leprosy reactions can quickly lead to permanent nerve damage with increased paralysis of the hands, feet, or eye muscles, or to permanent damage to the eyes.
| Early treatment of leprosy reactions is very important to prevent paralysis, deformity, and blindness. |
Treatment of leprosy reaction is discussed on Page 221.
TREATMENT AND MANAGEMENT OF LEPROSY
Treatment and management of leprosy include 4 areas.
- Long-term medical treatment to control the leprosy infection should begin as early as possible.
- Emergency treatment when necessary to control and prevent further damage from leprosy reactions.
- Safety measures, aids, exercises, and education to prevent deformities (sores, burns, injuries, contractures).
- Social rehabilitation: Work with the individual, the parents, the schools, and the community to create a better understanding of leprosy, to lessen people's fears, and to increase acceptance, so that the child or adult with leprosy can lead a full, happy, meaningful life.
Medical treatment
Medical treatment of leprosy varies according to the policies and resources of the particular country and health ministry. For years, DDS (dapsone) has been the main drug used. Unfortunately, in some areas the leprosy bacilli are becoming 'resistant' to DDS (are not harmed by it).
Rifampin usually works much faster against leprosy. However, it is more costly and can also cause serious side effects. Still, where possible, it should be used. To prevent development of resistance, it is usually given in combination with other anti-leprosy medicines. When given in combination with DDS, rifampin probably needs to be given only once a month. This reduces both cost and side effects.
Clofazimine, although less effective in killing leprosy bacilli than rifampin, has the advantage that it also helps control leprosy reaction.
Multi-drug treatment, consisting of rifampin, DDS, and clofazimine, is now recommended by the World Health Organization. It greatly reduces the time needed for treatment, especially for tuberculoid leprosy.
Instruction for the dosage and precautions for these different medicines should be obtained from the local leprosy control program. Usually it is wise to cooperate with these programs instead of trying to treat leprosy by yourself.
Importance of long-term treatment
Treatment to cure leprosy takes a long time: from 1 to 2 years or more, depending on the type of leprosy and the medicine used. If treatment is stopped too soon, not only can leprosy return, but sometimes a leprosy reaction may result which can cause even more nerve damage and paralysis or blindness.
It is therefore essential that health and rehabilitation workers make sure the person with leprosy and her family understand the importance of taking the medicines regularly.
Health centers should take care always to keep a reserve supply of medicines on hand.
| TREATED EARLY, LEPROSY NEED NOT BE A DEFORMING OR DISABLING DISEASE. |
Treatment of leprosy reactions
As we mentioned on Page 215, feeling loss, paralysis, and deformities need not happen to a person with leprosy.Early diagnosis and treatment together with quick care of leprosy reactions should prevent the development of many deformities.
Care of a leprosy reaction has 4 objectives:
-
Prevent nerve damage that causes loss of feeling, paralysis, and contractures.
-
Stop eye damage and prevent blindness.
-
Control pain.
-
Continue with medicine to kill leprosy bacilli and prevent the disease from getting worse.
Care includes:
-
Medicine to reduce pain and inflammation
For mild reactions (skin inflammation but not pain or tenderness of nerves) aspirin is the best and cheapest drug. For dosage and precautions, see Page 134.
Chloroquine (a medicine for malaria) is also effective. To adults, give 2 tablets of 250 mg. at night (to avoid dizziness) for no more than 2 or 3 weeks. Give less to children, according to their weight.
For severe reactions (pain along nerves, increasing tingling, numbness or weakness, eye irritation, or painful testicles)corticosteroids (prednisolone) may be needed. Because this is a medical emergency and because corticosteroids are dangerous and often misused medicines, if at all possible get experienced medical advice before using them.
-
Anti-leprosy medicine should be continued throughout the leprosy reaction.
Clofazimine can be used instead of DDS, as clofazimine helps to reduce reactions and fights the leprosy bacilli. The dose of clofazimine can often be increased (to 200 mg. daily in adults) and later reduced as the reaction lessens. However, for severe reactions that damage nerves, prednisolone is needed.
-
Splinting and exercise
Holding the affected limbs in splints during a severe reaction helps reduce pain and prevent nerve damage and contractures. (See Chapter 8.)
Joints should be splinted in the most useful position. Splints can be made of plaster bandage or molded plastic (see Page 540). Very carefully pad splints for hands or feet that do not feel pain.
Leave the splint on day and night until pain and inflammation are gone. Remove only for gentle range-of-motion exercise at least once a day. (See Chapter 42.)
Cause of deformities
When most people think of leprosy, they think of the severe deformities of the advanced case: deep open sores (ulcers), clawed fingers, gradual loss of fingers and toes, and eye damage leading to blindness. Actually, these deformities are not caused directly by leprosy germs, but result from damaged nerves. Nerve damage causes 3 levels of problems, one leading to the next:
|
LEVEL 1: loss of feeling, of sweating, and of strength in certain muscles
often PREVENTABLE with medical treatment of leprosy before there is nerve damage |
|
LEVEL 2: injuries, joint stiffness
often PREVENTABLE with protective eye and skin care and exercise to keep full movement of joints |
|
LEVEL 3: progressive deep infections with bone destruction and loss of vision
often PREVENTABLE with careful early treatment of sores, burns, and infections |
When there are level 1 problems, there is a lifelong danger of level 2 and 3 problems. Because feeling has been lost, the person no longer protects herself automatically against cuts, sores, thorns, and other injuries. And because they do not hurt, these injuries are often neglected.
For example, if a person with normal feeling walks a long way and gets a blister, it hurts, so he stops walking or limps.
|
But when a person with leprosy gets a blister, it does not hurt.
|
|
So he keeps walking until the blister bursts and becomes infected.
|
|
Still without pain, the infection gets deeper and attacks the bone.
|
|
In time the bone is destroyed and the foot becomes more and more deformed.
|
Usually, leprosy bacilli cannot be found in these open sores. This is because the sores are not caused by the bacilli. Instead, they are caused by pressure, injury, and secondary infection.
PREVENTION OF INJURY for persons with loss of feeling and strength
Eyes: Much eye damage comes from not blinking enough, because of weakness or loss of feeling. Blinking keeps the eyes wet and clean. If the person does not blink well, or his eyes are red, teach him to:
-
Wear sunglasses with side shades, and maybe a sun hat.
-
Close the eyes tightly often during the day, especially when dust blows.

-
Roll the eyeballs up as you try to close eyes tight.
-
Keep eyes clean. Wash well around eyes, keep flies and dirty hands away.
Hands: When you work with your hands, or cook meals, take special care. Never pick up a pan or other object that might be hot without first protecting your hand with a thick glove or folded cloth. If possible, avoid work that involves handling sharp or hot objects. Do not smoke.
-
Use tools with smooth, wide handles, or wrap cloth around handles.
To help the person with weak or deformed fingers hold a tool or utensil, you can mold a handle to the shape of the person's closed hand.
Use epoxy putty, or plaster of Paris mixed with a strong glue. Have the person grip the handle while it is still soft. Then let it harden.
Feet:
-
Avoid going barefoot. Use shoes or sandals. (For suggestions on appropriate footwear, see the next page.)
-
Learn to take short steps. This helps protect the feet.
INJURY CARE

Eyes: Close eyes often. If necessary, use a simple eye patch. If eye gets infected (forms pus) use an antibiotic eye ointment. Put the ointment into lower lid without touching the eye.
Hands and feet: If you have a cut or sore, keep the injured part very clean and at rest until it has healed completely. Take care not to injure the area again.
Things to do every day

-
Checkups: At the end of each day (or more often if you work hard or walk far) examine your hands and feet carefully-or have someone else examine them. Look for cuts, bruises, or thorns. Also look for spots or areas on the hands and feet that are red, hot, swollen, or show the start of blisters. If you find any of these, rest the hands or feet until the skin is completely normal again.

-
If the skin gets dry and cracks, soak the feet daily in water for at least 20 minutes. Then rub cooking oil, Vaseline, or lanolin hand cream into them (not butter or animal fat. These attract insects and rats).
-
As you rub oil into the hands and feet, do stretching exercises to keep the complete range of motion in the joints.
|
With continued daily care, most deformities of leprosy can be prevented. |
PREVENTION of contractures and deformities in persons with paralysis
Prevention of contractures from paralysis due to leprosy is similar to prevention of hand and foot contractures due to polio and other forms of paralysis. (See Page 81.) However, loss of feeling makes prevention more difficult.
Exercises to maintain full range of motion are covered in Chapter 42 (see especially Page 370 to 373).
-
Exercises to prevent fixed clawing of the hands can be done by ... ...
gently straightening the fingers like this:

and like this:

-
A good exercise to prevent 'tiptoe' contractures with 'foot drop' is to stretch the heel cords by leaning forward against a wall or by squatting with heels on the ground.
Footwear for persons without feeling in their feet
The best footwear has:

-
a well-fitted upper part that does not rub and has plenty of toe room (or leaves toes open).
-
a soft innersole about 1 cm. thick.
-
a tough under-sole so thorns, nails, and sharp rocks do not injure foot.
-
Footwear should be acceptable (not look too strange or unusual) so that the person will use it.
AVOID:
|
Possible ways to get footwear
-
Contact a leprosy hospital with a footwear workshop. They can make sandals if you send a tracing of the foot.

-
Check the market. You may find a canvas shoe or tennis shoe that already has a good insole.
-
Or you can put soft insoles into the shoes. But CAUTION: If you put an insole that is thick into a standard shoe, there may not be enough room for the toes - unless you cut out the part over the toes and leave them open.
-
Make (or have a local shoemaker make) special footwear.

For the inner sole, you can use a soft sponge sandal or 'thong'. Or buy 'microcell' rubber, which is soft but firm.
For the under-sole you can use a piece of old car tire.

-
For persons who have developed sores on their foot here,

a bar here or a foot support here may help take pressure off the ball of the foot and prevent new sores.

-
A very helpful lining for preventing sores is a soft, heat-moldable foam plastic called 'Plastazote'. For instructions on making footwear with Plastazote, see Insensitive Feet on Page 638.
-
For persons with a 'drop' foot, a brace or 'lift' can help prevent sores and injuries.

You can get a brace or support at a rehabilitation workshop, or make a specially-fitted, well-padded plastic brace (see Chapter 58).

Or make a simple device to hold the foot up.
LEPROSY AND THE COMMUNITY
Historically, there has been a lot of fear and misunderstanding about leprosy. Persons with leprosy have often been thrown out of towns or treated with cruelty. Until recently, governments took persons with leprosy away from their families and locked them up in special institutions or 'leprosaria'. All this added to people's fears.
Today, leprosy can be cured-without any deformities or disabilities if treatment is begun early. It can be treated in the home. The person can continue going to school or to work. Having leprosy need not disable the person physically or socially.
But in many communities fear and misunderstanding remain. Persons still refuse to admit - even to themselves - the early signs of leprosy. They delay in getting treatment until permanent deformities appear. The disease continues to be spread to others by those who are not yet treated. And so the myth and the fear of leprosy are kept alive.
To correct this situation will require the efforts of all health and rehabilitation workers, schoolteachers, religious and community leaders, families of persons with leprosy, and organizations of the disabled. These steps are needed:
1. Information and Education Schools, health centers, comics, radio, and television can be used to help educate the community about leprosy. Information should:
- try to lessen the fears people have about leprosy and let them know it is curable.
- stress the importance of early diagnosis and treatment.
- tell people how to recognize early signs and where to get treated.
- include popular stories of persons who think they might have leprosy, decide to get help, and are cured.
2. Integration of leprosy programs into general health care. Too often leprosy control is done as a separate program. It is important that people (and health workers) begin to see leprosy as 'just another serious health problem'- like diarrhea in children.
3. Regular screening (mass checkups) of children for skin patches and other early signs of leprosy. This can be part of a 'CHILD-to-child' program (see Chapter 47) in which school children learn first to examine each other, and then their younger brothers and sisters. A 'CHI LD-to- child Activity Sheet on Leprosy' is available from TALC. (See Page 427.)
4. Community pressure and government orders to let children being treated for leprosy attend school, find work, attend festivals, and take part in public functions. (Organizations of disabled persons can help make this happen.)
5. Community support groups to help persons with leprosy feel accepted, cared for, and respected; also to make sure that they take their medicines regularly and learn to prevent deformity. Where needed, support groups can help persons with leprosy get the schooling, health care, work, and social rights they deserve.
|
The example of a health worker who welcomes persons with leprosy and is not afraid to touch them can do much to calm needless fears and encourage acceptance. |
Disabled Village Children
A guide for community health workers,
rehabilitation workers, and families
by David Werner
Published by
The Hesperian Foundation
P.O. Box 11577
Berkeley, CA 94712-2577