Disabled Village Children
A guide for community health workers,
rehabilitation workers, and families
PART 1
WORKING WITH THE CHILD AND FAMILY:
Information on different Disabilities
B. Recognizing, Helping with, and Preventing Common Disabilities
CHAPTER 23
Spinal Cord Injury
Spinal cord injury usually results from an accident that breaks or severely damages the central nerve cord in the neck or back: falls from trees or mules, automobile accidents, diving accidents, bullet wounds, and other injuries. Spinal cord injury is more common in adults and older children - and in many cultures it is twice as common in men as in women.
The spinal cord is the line of nerves that comes out of the brain and runs down the backbone (see Page 35). From the cord, nerves go out to the whole body. Feeling and movement are controlled by messages that travel back and forth to the brain through the spinal cord. When the cord is damaged, feeling and movement in the body below the level of the injury are lost or reduced.
Level of the injury
How much of the body is affected depends on the level of the injury along the backbone. The higher the injury is, the greater the area of the body that is affected.
The backbone consists of: 7 neck bones (cervical vertebrae), 12 upper back bones (thoracic vertebrae), 5 lower back bones (lumber vertebrae), 5 joined hip or sacral vertebrae, tailbones.
|
Quadriplegia:
|
|
Paraplegia:
|
Complete and incomplete injuries
When the spinal cord is damaged so completely that no nerve messages get through, the injury is said to be 'complete'. Feeling and controlled movement below the level of the injury are completely and permanently lost. If the injury is 'incomplete', some feeling and movement may remain. Or feeling and controlled movement may return (partly or entirely) little by little during several months. In incomplete injuries, one side may have less feeling and movement than the other.
X-rays often do not show how complete a spinal cord injury is. Sometimes the backbone may be badly broken, yet the spinal cord damage may be minor. And sometimes (especially in children) the X-ray may show no damage to the backbone, yet the spinal cord injury may be severe or complete. Often, only time will tell how complete the injury is.
EARLY QUESTIONS THAT A SPINAL CORD INJURED CHILD AND FAMILY MAY ASK
"Will my child always remain paralyzed?"
This will depend on how much the spinal cord has been damaged. If paralysis below the level of the injury is not complete (for example, if the child has some feeling and control of movement in her feet) there is a better chance of some improvement.
Usually the biggest improvement occurs in the first months. The more time goes by without improvement, the less likely it is that any major improvement in feeling or movement will occur.
Occasionally surgery to release pressure on the spinal cord or nerves, if done in the first hours or days following the injury, will bring back some movement or feeling. But surgery done more than a month after the injury almost never brings back any movement or feeling. Never agree to such surgery unless at least 3 independent and highly respected neurosurgeons recommend it.
After one year, the paralysis that remains is almost certainly there to stay. As gently as you can, help both the child and parents accept this fact. It is important that they learn to live with the paralysis as best they can, and not wait for it to get better or go from clinic to clinic in search of a cure.
|
It is best to be honest with the child and the family. Explain the facts of the situation as clearly, truthfully, and kindly as possible. |
"My child's feet are beginning to move! --spasticity
Immediately after a spinal cord injury the paralyzed parts are in 'spinal shock', and are loose or 'floppy'. Later (within a few days or weeks) the legs may begin to stiffen-especially when the hips or back are straightened. Also, when moved or touched, a leg may begin to 'jump' (a rapid series of jerks, called 'clonus').
This stiffening and jerking is an automatic reflex called 'spasticity'. It is not controlled by the child's mind, and often happens where spinal cord damage is complete. It is not a sign that the child has begun to feel where he is touched or is recovering control of movement.
|
CAUTION: Sudden jumping or stiffening of the legs when moved or touched does not mean feeling or controlled movement is returning. This is a spastic reflex.
|
Some children with spinal cord injury develop spasticity; others do not.
|
If the spinal cord injury is above the level of the top edge of the hipbone (above the 2nd lumbar vertebra) spasticity is very likely.
If the injury is below this level, paralysis is usually floppy (no muscle spasms). |
|
Severe spasticity often makes moving and control more difficult. However, the child may learn to use both the reflex jerks and spastic stiffness to help her do things. For example, |
 When the child wants to lift her foot, she hits her thigh, triggering the jerks that lift the leg. |
 In lower back injuries, the spasticity or stiffness of the legs may actually help the child stand for transfers. |
"Will my child be able to walk?"
This will depend mostly on how high or low in the back the injury is. The lower the injury, the better the chance of walking. A person with complete spinal cord injury in the neck has no chance of walking. She will need a wheelchair.
If the child's injury is in the lower back and if his arms are strong and he is not too fat, there is a chance he may learn to walk with crutches and braces. But he will probably still need a wheelchair to go long distances.
However, it is best not to place too much importance on learning to walk. Many children who do learn to walk find it so slow and tiring that they prefer using a wheelchair.
It probably makes sense to give most paraplegic children a chance to try walking. However, do not make the child feel guilty if he prefers a wheelchair. Let the child decide what is the easiest way for him to move about.

For independent living, other skills are more important than walking, and the family and child should place greater importance on these: skills like dressing, bathing, getting into and out of bed, and toileting. Self-care in toileting is especially important - and is more difficult because of the child's lack of bladder and bowel control.
"What are the hopes for my child's future?"
The chances of a paraplegic's leading a fairly normal life are good-provided that you:
- 1. avoid 3 big medical risks:
- · skin problems (pressure sores)
- · urinary infections
- · contractures (shortening of muscles, causing deformities)
(Contractures are not a danger to life but can make moving about and doing things much more difficult.)
- 2. help the child to become more self-reliant:
- · home training and encouragement to master basic self-help skills such as moving about, dressing, and toileting.
- · education: learning of skills that make keeping a household, helping other people, and earning a living more possible
It is more difficult for quadriplegic persons to lead a normal life because they are more dependent on physical assistance. However, in some countries many paraplegics and quadriplegics manage to lead full, rich lives, earn their own living, get married, and play an important role in the community. With effort and organization, the same possibilities can exist in all countries.
"Can anything be done about loss of bladder and bowel control?"
Yes. Although normal control rarely returns completely, the spinal cord injured child often can learn to be independent in his toilet, and to stay clean and dry (except for occasional accidents). Often he will need a special urine collecting device, will learn to use a catheter, and will learn to bring down a bowel movement with a finger or suppository. Management of bladder and bowels are discussed in Chapter 25.
| VERY IMPORTANT INFORMATION ON URINE AND BOWEL CONTROL IS IN CHAPTER 25. BE SURE TO READ THIS CHAPTER! |

"What about marriage, sex, and having children?"
Many spinal cord injured persons marry and have loving, sexual relationships. Women with spinal cord injuries can become pregnant and have normal babies. Men may or may not be able to get a hard penis or ejaculate (release sperm). Paraplegic and quadriplegic men whose injuries are incomplete are more likely to have children. Some couples where the husband cannot release sperm decide to adopt children. Whether or not they can have children, male and female spinal cord injured persons often enjoy loving sexual relationships.
Especially for young men, fear of the loss of sexual ability is often one of the most fearful and depressing aspects of spinal cord injury. Honest, open discussion about this, and the possibilities that do exist, with a more experienced spinal cord injured person may help greatly. There is a good discussion of this in Spinal Cord Injury Home Care Manual. See reference, Page 639.
HELPING THE CHILD AND FAMILY ADJUST
Spinal cord injury, especially in the child, brings many of the same problems as does spina bifida. Also many aspects of rehabilitation are similar. (We suggest you read Chapter 22 on spina bifida to get additional ideas for the rehabilitation of young children with spinal cord injuries.)
Perhaps the biggest difference from spina bifida is that spinal cord injury begins later. One day the child is physically active and able, the next he is suddenly paralyzed and (at first) unable to do much for himself. He has lost all feeling and control in part of his body; it is like a dead weight.
This is very hard for the child - and family - to accept. Both have an enormous fear and uncertainty about the future. The child may become deeply depressed, or angry and uncooperative. He may refuse even to sit in a wheelchair because this means accepting not being able to walk.
There are no easy answers to the child's fear and depression, but here are some suggestions families have found helpful.
-
Recognize that the child's fear, depression, and anger are natural responses and that with love, understanding and encouragement, he will little by little overcome them.
-

Be honest to the child about her disability. Do not tell her, "We will find a cure for you," or, "Soon you will get well and be able to walk again." Very probably this is not true, and telling the child such things only makes it more difficult for the child to accept her disability and to begin shaping a new life. Also, as the promised 'cure' fails to happen, the child becomes more uncertain, distrustful, and afraid. In the end, it wil be much easier for her if you gently tell the truth. Here is one example
-
Provide opportunities to keep the child's mind active: playing, working, exploring, learning through stories, games, and studies. But at the same time respect and be supportive of the child when he feels sad and frightened. Let him cry, comfort him when he does, but do not tell him not to cry. Crying helps relieve fear and tension.
-
Start the child with exercises, activities, and relearning to use her hands and body as soon as possible. Start with what the child can do, and build on that.
-
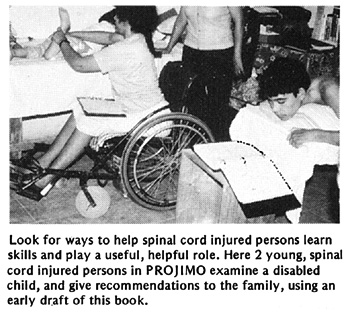
Try to have the child watch, talk with, and get to know other persons with spinal cord injury (or children with spina bifida), especially those who are living full and happy lives.
-
Invite the child's friends to come visit her, play with her, and let her know that they are eager for the day she will be back in school.
-
Encourage the child to do as much for herself as possible. Let her do anything she can do for herself - even if it takes longer.
Help in ways that let the child do more for herself. -
As much as possible, avoid 'tranquilizers' or other strong medicines. The child needs an alert mind and an ability to move actively all day.
HOW TO PREVENT MORE SEVERE SPINAL CORD INJURY IN CASE OF ACCIDENT
When a person has just had an accident that may have injured the spinal cord, great care must be taken to prevent further damage.
After an accident, there may be spinal cord injury if:
-
the person is unconscious, or
-
the person cannot move, cannot feel, or has numbness in his legs or hands.
If you think the spinal cord might be injured:
-
Do not move the person until a health worker with a large board or stretcher arrives. Especially avoid bending the person's neck and back.

-
Lift the person without bending him, onto a board or stiff stretcher. (A stiff rack is better than a soft stretcher. Make one out of poles from trees or whatever is available.) Make ties of strips of clothing, or whatever you can.
-
Tie him down firmly and stabilize his head.
-
Carry the person to a medical center or hospital. Try not to bounce or jiggle him.
HOW TO LIFT A SEVERELY INJURED PERSON ONTO A STRETCHER
from Where There Is No Doctor
|
1. With great care, lift the injured person without bending him anywhere. |
|
2. Make sure that the head and neck do not bend. Have another person put the stretcher in place |
|
3. With the help of everyone, place the injured person carefully on the stretcher. |
|
4. If the neck is injured or broken, put bags of sand or tightly folded clothing on each side of the head to keep it from moving. |
Common secondary problems in children with spinal cord injury
Page 190., Page 178., Page 187., Page 184., Chapter 24., Page 182., Page 185., Page 186., Page 176., Page 184.
To prevent or reduce the harmful effects of these problems, special precautions need to be taken early and continued throughout life.
EARLY CARE FOR THE SPINAL CORD INJURED PERSON
Early care following spinal cord injury is best done in a hospital, especially if the child is likely to get good nursing care. Family members should stay with the child in the hospital to make sure the child is kept clean and turned regularly, so that bed sores and pneumonia are avoided. (Busy hospital staff with little experience treating spinal cord injuries sometimes let severe bed sores develop-which may threaten the child's life.)
|
CAUTION: During the first 6 weeks, or until any breaks in the bone have healed, take great care when turning the child so that the angle of his back, neck, and head does not change. Use the same methods and precautions used in lifting a newly injured person onto a stretcher (see Page 180). When the neck or back has healed, the child can start lying on his stomach, at first for 10 minutes and then longer if there are no problems. |
Surgery of the spine may or may not be necessary. After surgery, the person must lie very still for at least 6 weeks. The main purpose of surgery is to prevent more damage-not to cure the paralysis. The damage already done to the spinal cord cannot be corrected with surgery or medicine.
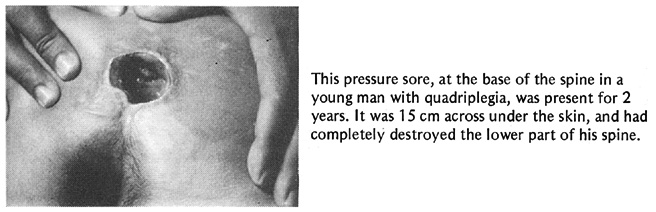
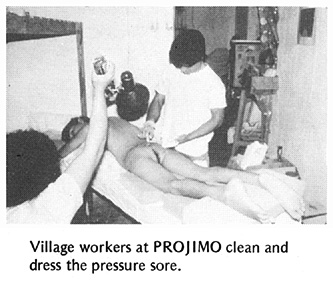
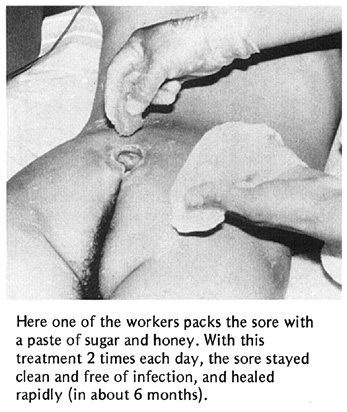
Preventing pressure sores (bed sores)
When feeling has been lost, pressure sores can easily form on the skin over bony areas - especially on the hips and butt. The biggest risk of sores is in the first weeks after the injury. This is because the child must stay very still, and has not yet learned to move or turn over his body. Prevention of pressure sores is extremely important, and needs understanding and continuous care, both by the child and those caring for him.
|
BE SURE TO READ CHAPTER 24 ON PREVENTION AND TREATMENT OF PRESSURE SORES. |
Summary: early prevention of pressure sores (For details, see Chapter 24.)
- Lie on a soft mattress or thick, firm, foam rubber pad.
- Place pillows and pads to keep pressure off bony areas.
- Change position (turn over from front to back and side to side) every 2 to 3 hours. To avoid pressure sores, lying on the belly is the best position).
- Keep skin and bedclothes clean and dry.
- Eat good food rich in vitamins, iron, and protein.
- Move and exercise a lot to promote good flow of the blood.
Check skin daily for earliest signs of pressure sores-and keep all pressure off beginning sores until the skin is healthy again.
Avoiding contractures
In the first weeks following a spinal cord injury, when the child is in a lying position, joint contractures (muscles shortening) can easily develop, especially in the feet and elbows. Pillows and pads should be placed to keep the feet supported, the elbows straight, and the hands in a good position. Gentle range-of-motion exercises of the feet, hands, and arms should begin as early as possible, taking care not to move the back until the injury is healed. Further discussion on the prevention of contractures in the spinal cord injured is on Page 184.
PHYSICAL THERAPY FOLLOWING SPINAL CORD INJURY
ASSISTED BREATHING AND COUGHING
Persons with spinal cord injury in the neck or upper back often have part of their breathing muscles paralyzed. Slowly the remaining muscles become stronger and breathing improves. But breathing often stays weak. The person may not be able to cough well and can more easily get pneumonia.
To help the person cough, place hands as shown below. Ask him to cough, and as he does, push firmly inward on the chest. Be careful not to move the backbone.

TWO-PERSON ASSISTED COUGH
Do this several times a day when the person has a cold, and more often if the person develops more trouble breathing or seems to have a lot of mucus in his lungs or throat.
ONE-PERSON ASSISTED COUGH
To help the child breathe deep and to stimulate the breathing muscles, press lightly here while the child tries to breathe deeply in and out.
Do this for a few minutes, several times a day.

If the person has a lot of mucus in her lungs, it also helps to lie her down, like this, and pat her back briskly. This helps loosen the mucus so that it can be coughed out. Be sure she drinks lots of water to help loosen the mucus.
MOVEMENT AND EXERCISE
Do range-of-motion exercises for about 10 minutes for each arm and leg. In the first weeks, do the exercises twice a day. Later, once a day may be enough. If any signs of contracture develop, spend more time and effort on those parts of the body. From the start, exercises should be bothpassive (someone else moves the child's body parts) and whenever possible, active (the child does it himself).
Range-of-motion exercises should begin with great care the day after the spine is injured (see Chapter 42). The exercises will help to improve the flow of blood (which reduces the chance of bed sores), to prevent contractures, and to build the strength of the muscles that still work. Range-of- motion exercises should be continued throughout life, when possible as a part of day-to-day activity.
CAUTIONS:
-
Until any breaks or tears in the spine have healed (6 weeks or more) exercise must be very gentle and limited, with smooth motions and no jerking.
– Especially at first, take great care that exercises do not move the position of the back and neck. Start with feet, ankles, hands, wrists, and elbows.
– If exercises trigger severe muscle spasms or jerking, do not do them until the break is healed.
Do not use force in trying to get the full range of motion, as joints can easily be damaged
.
For quadriplegics often it is better to stretch the fingers only when the wrist is bent down like this,
but not when it is bent back like this.
This way enough contracture is left to be useful for taking hold of things. Although the fingers lack movement by muscles, they close around an object when the wrist is bent back.
If possible, get instructions from an experiencedphysical therapist
-
Try to keep the full range of motion of all parts of the body. But work most with those joints that are likely to develop contractures, especially:
Prevent this through exercises (see Page 383) and by supporting feet (Page 184.)– paralyzed parts that tend to hang in one position, such as the feet,
– or, joints that are kept straight or bent by spasticity or by muscle imbalance (see Page 78). For example:

In quadriplegia the muscles that straighten the elbow are usually paralyzed, while the muscles that bend the elbow stay fairly strong. These muscles keep the elbow bent, and in time they shorten so that the arm can no longer straighten fully. |

It is important that the arms can straighten until they bend backward a little - which is the only way he can lift himself with his arms. |
|
For this reason, straight arm positioning and early range-of-motion exercises for the elbow are essential. While he is still kept lying down, teach him to straighten his elbows by turning his hands up and then lifting his arms.
|
MAINTAINING HEALTHY POSITIONS
The position that the body is in during the day and night is also important to prevent contractures.
Contractures that cause 'tiptoeing' of the feet can develop easily, especially when there is spasticity. Keep the feet in a supported position as much of the time as possible:


when lying down, and when sitting.
|
CAUTION: A support like this works well with floppy feet, but may trigger spasticity or jerking of the feet. Position them slowly. |
Teach the child to make sure his feet are in a good position.
Even for the child who may never walk, maintaining the feet in a flat position makes moving from chair to bed, toilet or bath easier.
Another common problem for children with spasticity is that the knees pull together and in time contractures prevent the legs from separating. To prevent this, when the child lies on her side she should learn to


place a pillow between the legs, and to keep it there most of the time.
A common problem with wheelchair users is that they slump forward. In time this can deform the spine.
|
In a wheelchair with a straight-up back a person with spinal cord injury slumps like this in order to balance.
|
|
A chair can be designed (or adapted) so that it tilts back. This provides balance for a better position.
|
|
A special cushion also helps keep the butt from sliding forward (and helps prevent pressure sores).
|
For more suggestions for wheelchair adaptations, see Chapters 64 and 65. For more ideas on cushions, see Page 199 and 200.
EARLY PHYSICAL RE-EDUCATION
The goal for a spinal cord injured person is to become as independent as possible in doing what he or she wants and needs to do. But even before the skills of daily living are relearned, the person needs to learn to protect the body where functions that used to be automatic have been lost. The protective functions that may be lost or changed include:
- Adjustment of blood pressure to changes in body position.
- Feeling (including pain) that protects from injuries (such as bed sores).
- Sense of body position and ability to keep balance.
- Muscle strength and coordination.
- Control of body temperature-especially keeping cool in hot weather.
1. A sudden drop of blood pressure in the brain when the person rises from lying to sitting, or sitting to standing, can cause dizziness or fainting. This is a common problem in spinal cord injury because the blood pressure adjustment mechanism is partly lost. Little by little the body can be helped to re-adapt, but precautions are needed. (These same precautions are for anyone who has been kept lying down a long time.)
|
Before beginning to sit, raise the head of the bed - a little more and a little longer each day.
In a week or 2 build up to this for 3 hours. |
If the person begins to get dizzy or faint when sitting, tilt him back and lift his feet. |
|
Lifting exercises help the body relearn to adjust blood pressure - and also prevent bed sores and strengthen arms.
|
Before beginning to stand, make a standing board, and strap the child to it. Start at a low angle, and stand the board up more -and longer- each day.
|
2. The loss of feeling in parts of the body can lead to pressure sores and other injuries, such as burns and cuts. This is because the body no longer feels pain and does not warn the child to change position or move away from danger.
It is important that the child learn to protect himself by changing positions often and avoiding injuries. This includes:

|
|
|


|
Keeping clean is very important for persons with reduced feeling, especially if they lack bladder and bowel control. Take care to bathe daily. Wash and dry the genitals, the butt, and between the legs as soon as possible each time they get wet or dirty.
If redness, diaper rash, or sores develop, wash more often and keep the sore area dry. Keep the legs spread open and exposed to the air. When they must be covered, use soft absorbent cotton cloth. Putting a little vinegar in the rinse water after bathing the child, and after washing diapers and underclothes, helps prevent skin rash and infection.
For treatment of specific skin infections (fungus, yeast, bacteria) consult a health worker or a medical book (like Where There Is No Doctor, see Chapter 15).
3. Loss of ability to sense what position the body is in affects a person's sense of balance. So does loss of muscle control. The child needs to develop new ways to sense the position of his body and keep his balance. Start with the child sitting on a bench, if possible, in front of a mirror.
Help the child progress through these stages:
-
both hands on bench
-
both hands on knees
-
lift one arm sideways, forward, and back
-
After doing this in front of a mirror, have him do it without the mirror.

- As the child gains better balance, start doing different movements with first one and then both arms, such as lifting weights or playing ball.
|
Note: Some children may have so much difficulty with balance that they may have to start in a wheelchair or a chair with high back and arm supports. |
4. Muscle re-education All muscles that still work need to be as strong as possible to make up for those that are paralyzed. Most important are muscles around the shoulders, arms, and stomach.
5. Temperature control Normally, when a person feels hot, he sweats and the blood vessels beneath the skin swell. This automatic cooling system is partly lost in persons with high spinal cord injury. In hot weather, they may get high fever or can even die of heat stroke.
|
For this reason they must learn (and be allowed) to rest quietly in the shade, in the coolest place possible, during the hottest part of the day.
|
|
|
|
Children with spinal cord injury can learn to paddle around very well in old tire tubes. They love it, and it is excellent arm and shoulder exercise. However, it is very important that someone watches them.
|
| TAKE CARE also to protect against cold. Body temperature can also drop too low. |
DYSREFLEXIA (Sudden high blood pressure with pounding headaches)
Persons with quadriplegia or very high paraplegia run the risk of 'dysreflexia'-or sudden, dangerous increase in blood pressure with severe pounding headaches.
Dysreflexia is the body's reaction to something that would normally cause pain or irritation, but which the person does not feel because of the spinal cord injury.
|
COMMON CAUSES OF DYSREFLEXIA
SIGNS (OF DYSREFLEXIA)
|
|
Dysreflexia is a medical emergency. The high blood pressure could cause fits or deadly bleeding inside the brain. |
What to do
Act quickly to remove the cause and lower the blood pressure.
-
Quickly lower the blood pressure in the head.
– If lying, sit up ; stay sitting until the signs go away.
– Change position, drop feet down, loosen belt or straps, remove tight stockings.
-
Look or the cause of Dysreflexia, and remove it if possible.
– Bladder. Feel the lower belly to see if the bladder is full. If a catheter is in place, check for bends or kinks and straighten them to let urine flow. If the catheter is stopped up, open it by injecting 30 cc. of boiled and cooled water (or sterile saline solution) into the catheter. Or take the catheter out. If a catheter is not in place and the person cannot pee, put in a catheter and empty the bladder (see Page 206).
– If urinary infection appears to be the cause, inject an anesthetic solution into the bladder through a catheter. Use 10cc. 1 % lidocaine in 20cc. of boiled water. Clamp the catheter for 20 minutes and then release. Treat the infection (see Page 210).
Bowel. If the bladder does not seem to be the cause, check for a full bowel. How long has it been since the last bowel movement (shit)? Put some lidocaine (Xylocaine) jelly on your finger and check if the bowel is packed with hard shit. If it is, put in more lidocaine jelly. Wait 15 minutes, or until the headache becomes less. Then gently remove the shit with your finger.
– Pressure. Change the child's position in order to relieve pressure over bony areas. (Sometimes just staying in the same position too long can bring on dysreflexia.)
-
It the signs do not go away, get medical help as fast as possible.
-
If the child has frequent or severe periods of dysreflexia, or you cannot find the cause, try to have him seen by a specialist on spinal cord injury, and possibly a 'urologist' (specialist of the urine system).
|
Suggestion: For quadriplegics in villages, it is wise to have injectable 1% lidocaine (Xylocaine) and lidocaine gel available for dysreflexia emergencies. |
Self-care
With help and encouragement of family, friends andrehabilitation workers, the child with spinal cord injury can learn to become as independent as possible in meeting his basic needs: moving about, eating, bathing, dressing, toileting, and in time other skills for daily living.
Progress toward self-care, especially at first, may be slow and frustrating. The child will need a lot of understanding and encouragement. Persons with low spinal cord injury will find it easier to relearn self-care skills than those with higher injuries who have less use of their hands and arms. Quadriplegics usually will remain at least partly dependent on others for some of their daily activities. To make activities easier both for themselves and their helper, it is important that they avoid getting fat.
Useful methods and techniques have been worked out for helping relearn basic skills. We cannot describe many of these in detail. However, much depends on determination, imagination, and common sense. Start with first things first-like rolling over and sitting up in bed.
A few simple aids can often help a person become more independent. For example,
 (See Page 199.)
(See Page 199.)
When hands are affected, devices like these (or others that you can invent) make relearning to eat and write easier.
'Velcro' sticks-to-itself tape makes it possible for the person to put on aids by herself.
For additional ideas of aids for self-care, see pages 571 to 578. Suggestions for getting in and out of wheelchairs and learning to walk with crutches are included in Chapter 43.
KEEPING ACTIVE

Many of the 'complications' of spinal cord injury happen because the person spends a lot of time just lying and sitting. To keep healthy, the body needs to keep active. Lack of movement and activity causes poor flow of the blood. This can lead to pressure sores, swollen feet, painful or dangerous blood clots (thrombosis) especially in the legs, increasing weakness of bones (osteoporosis) with risk of breaking them, stones in the bladder or kidneys, increased risk of urinary infections, and general physical weakness and poor health.

It is important -both for the body and mind- that spinal cord injured persons keep physically active. Let your child do as much for herself as she can: pushing her own wheelchair, bathing, transferring, washing clothes, cleaning house, and helping with work.
Active games and sports can also be encouraged. Swimming, basketball, and archery can be done well with upper body use only.
Quadriplegics can become skillful with bow and arrow by using a straight-arm splint and a special hook, fastened to the hand, to pull the string.
(Note: Archery may also help correct spinal curve. The arm that pulls the string should be on the side with bulge in the back.)
To keep leg bones growing well and to prevent them from becoming weak and breaking easily, even children who may always be wheelchair riders should stand for a while every day. Standing also helps the child's bowels move more often.

This can be done by strapping the child to a 'standing board', or by making some kind of a standing frame.
This standing frame was invented by a paraplegic youth and his father. The boy uses the spasticity in his legs to stand. When the muscles tire he hangs and sits on the padded poles.
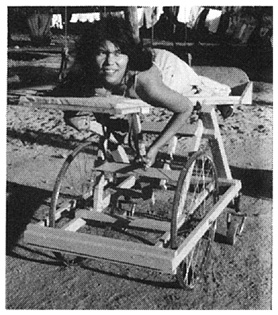
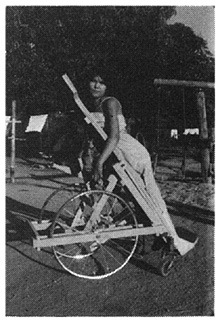
This design for a standing wheel-bed allows a spinal cord injured child with pressure sores on her butt to actively move about. The child can adjust it while on it, from a flat-lying position to a near-standing position. It can be made out of wood or metal.
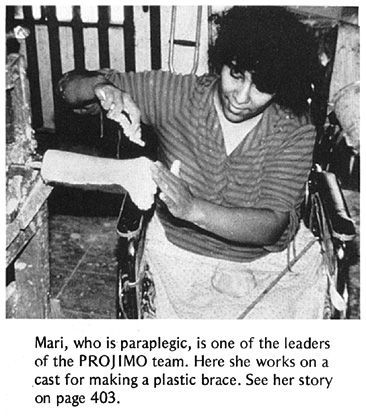
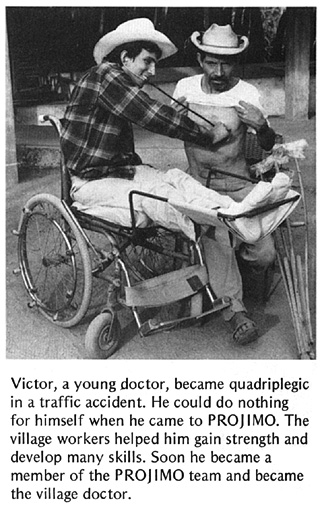
Spinal cord injured persons as leaders
Spinal cord injured persons in various countries are now taking the lead in making new lives for themselves and in getting their communities to recognize their abilities. Examples of 2 programs run primarily by spinal cord injured persons are included in Chapter 55. These are the Organization of Disabled Revolutionaries in Nicaragua (Page 519) and the Centre for the Rehabilitation of the Paralysed in Bangladesh (Page 518). Members of these and many similar organizations would be happy to share ideas and suggestions with any group of disabled persons interested in organizing their own program or shop.
OTHER PARTS OF THIS BOOK WITH INFORMATION USEFUL FOR SPINAL CORD INJURY
|
IMPORTANT: In addition to this chapter, some essential information for spinal cord injury is in other parts of this book, especially Chapter 24,"Pressure Sores," and Chapter 25, "Urine and Bowel Management!" These chapters are a continuation of information on spinal cord injury. We have put them in separate chapters because the information they cover is also essential for other disabilities. |
Chapters marked with a star (*) are essential for basic care of spinal cord injury.
*Chapter 24 Pressure Sores
*Chapter 25 Urine and Bowel Management (includes urinary infections)
Chapter 26 Leprosy (especially Page 223 to 225 on advice for care of hands and feet without feeling)
Chapter36 Feeding, especially aids for feeding, Page 330 to 332
Chapter 37 Dressing
Chapter 38 Toilet Training, especially aids, Page 342 to 344
Chapter 39 Bathing
*Chapter 42 Range-of-motion and Other Exercises
*Chapter 43 Crutch Use, Cane Use, and Wheelchair Transfers
Chapter 51 Adapting Home and Community to Needs of the Disabled
Chapter 52 Growing Up, Social Adjustment, Love, Sex, Role in Family and Community
Chapter 55 Example 3, Centre for the Rehabilitation of the Paralysed, and Example 4, Organization of Disabled Revolutionaries
Chapter 58 Braces
Chapter 63 Walking Aids
Chapters 64,65,66 Wheelchairs
For other references to spinal cord injury, see the INDEX, Page 652, and the books and reference materials listed on Page 638.
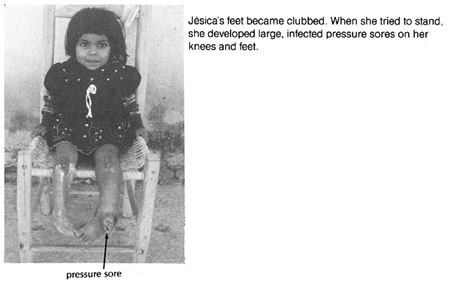
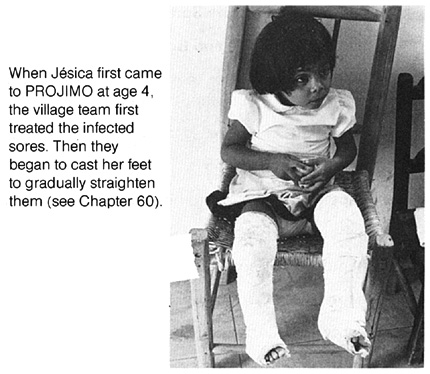
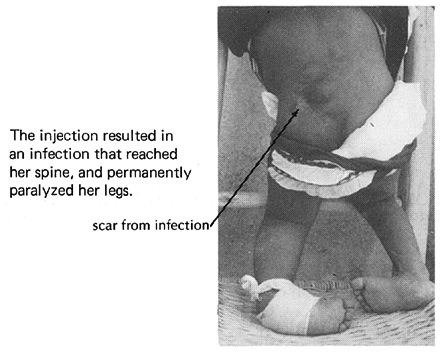
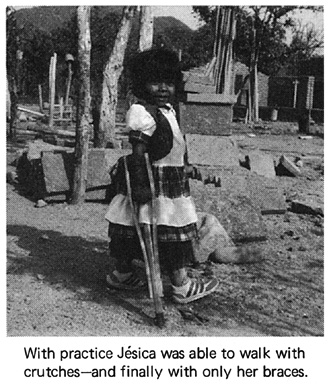
THE STORY OF JÉSICA
Jésica is a little girl who was paralyzed because of an unnecessary injection she received when she was 3 days old. Her mother does not know why or with what she was injected. This is the story of her rehabilitation at PROJ1IMO.
|
Misuse of medicines and especially injections is a common and preventable cause of disability. See Chapter 3. |
|
|
|
See Chapter 60 |
|
|
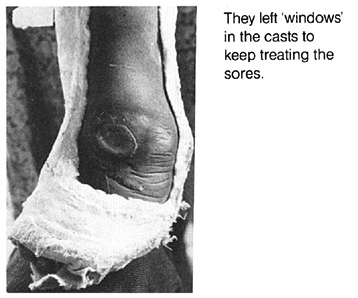
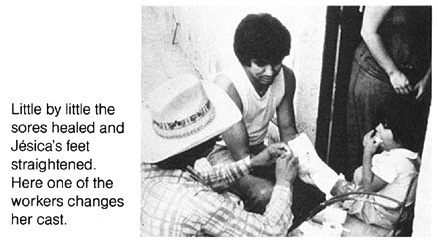
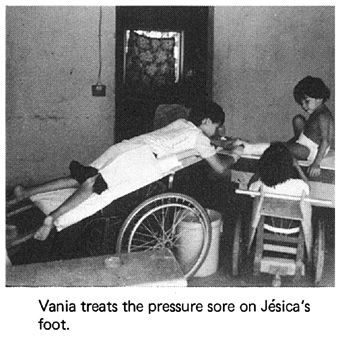
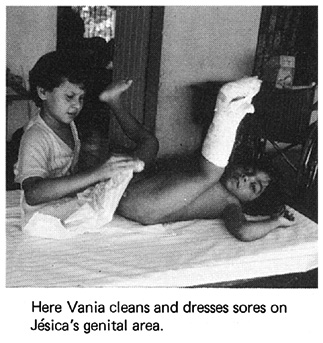
Jésica also lacks normal bowel and bladder control. From the uncontrolled loss of urine, she developed pressure sores in her genital area. Vania, an 8-year-old paraplegic girl, helped treat Jésica's sores. She also assisted Jésica with a 'bowel program', which helps her 'time' her bowel movements (see picture on Page 212). This makes daily activities and going to school much easier.
|
|

|
|
Jésica now goes to school in the village. Seeing disabled persons at PROJIMO who were happy, active, and accepted in the community has given Jésica a more hopeful, confident, and adventurous outlook on life.
Disabled Village Children
A guide for community health workers,
rehabilitation workers, and families
by David Werner
Published by
The Hesperian Foundation
P.O. Box 11577
Berkeley, CA 94712-2577










 Start like this for 15 minutes.
Start like this for 15 minutes.